This section provides an overview of the following topics regarding Reconciliation:
What Is Reconciliation?
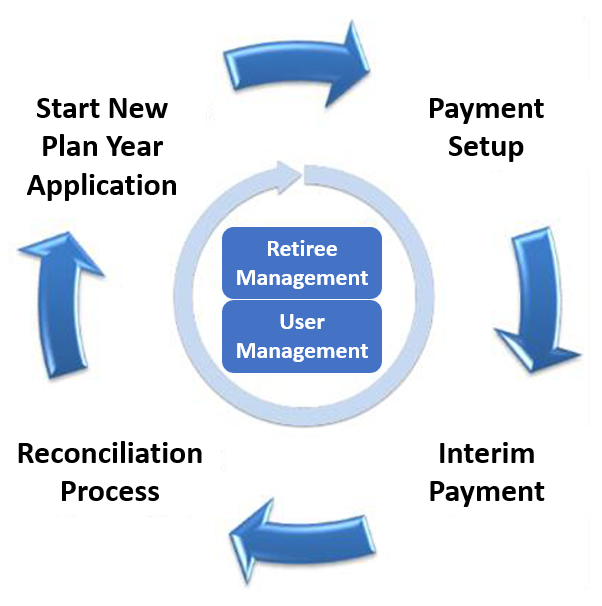
Application Lifecycle
Reconciliation is a part of an application's lifecycle. This cycle includes the following stages:
Within the lifecycle, User Management and Retiree Management are ongoing processes.
This figure shows how Reconciliation fits into the application lifecycle.
Reconciliation is the final stage of the application lifecycle that Plan Sponsors are required to complete for each application after the plan year has ended. In Reconciliation, a Plan Sponsor reports the total gross covered retiree plan-related prescription drug costs, including Actual Cost Adjustments (for example, discounts, chargebacks, rebates, and similar price concessions) for a specific plan year.
All Benefit Options for which an interim payment has been made within an application must be included in the Reconciliation payment request. The sum of the interim payments is then compared with the final subsidy payment determination for the application. If the sum of the interim payments is larger than the final subsidy payment request for the application, CMS initiates immediate overpayment recovery action, which may include collection of overpayment remittance in the form of a check or money order or offset against another application. For more information, refer to Satisfy an Overpayment.
Plan Sponsors that did not receive any interim payments and wish to receive subsidy must use the Reconciliation process to submit final cost reports and submit their one and only subsidy payment request for the plan year. This request consists of the total gross covered retiree plan-related prescription drug costs, Threshold Reduction, Limit Reduction, and Actual Cost Adjustments for the application.
All RDS applications have a maximum payment frequency of monthly interim payments, consistent with the general payment rules regarding timing set forth in 42 C.F.R. 423.888(b)(1). Although 12 interim payment requests are permitted, a Plan Sponsor may choose to submit fewer than 12 interim payment requests, or forego interim payments and instead choose to submit one final payment request during Reconciliation as described in 42 C.F.R. 423.888(b)(2)(ii).
Timing & Dependencies
Reconciliation is available in the left Navigation Menu of the Application as "View Only" after application approval and any time before Reconciliation is initiated. Reconciliation cannot be initiated until after the application has been submitted and approved AND the application plan year ends. Individual Reconciliation steps become active when the Plan Sponsor initiates Reconciliation and remain active until the Plan Sponsor completes Reconciliation or until the Reconciliation Deadline date has passed.
A Plan Sponsor is required to complete Reconciliation or submit a final payment request for each application for which they are seeking subsidy. The Reconciliation process should be completed using the RDS Secure Website by the Reconciliation Deadline date.
For a general table of Reconciliation Deadline dates by Plan Year End Date and important Reconciliation information, refer to Important Reconciliation Deadline Information.
Each application is reconciled individually and must be reconciled by the applicable Reconciliation Deadline. The Reconciliation process for a given application is independent of any other applications for that Plan Sponsor. Interim cost reports and interim payment requests should continue to be submitted for applications not being reconciled.
Reconciliation can typically average 90 days to complete. Reconciliation requires the Plan Sponsor to thoroughly prepare, allocate, align, and review all necessary resources required to complete each process step prior to submitting a final payment request. A successful Reconciliation is often one in which the Plan Sponsor identifies one individual to coordinate completion of all Reconciliation steps. For more information, refer to the Reconciliation Toolkit.
System Constraints: Is My Application Ready for Reconciliation?
An RDS application is ready for Reconciliation when the following conditions are met.
- The application is approved.
- The application plan year has ended.
- All desired interim payment requests have either been processed or canceled. The maximum number of interim payment requests does not have to be used before initiating Reconciliation. However, Plan Sponsors should not begin Reconciliation if they intend to submit further interim payments.
Note: A Plan Sponsor cannot have a negative interim payment request when they start Reconciliation. If there is a negative interim payment, and it will not be fully offset by a positive payment request on another application, the Plan Sponsor needs to contact CMS’ RDS Center to initiate the cancellation process.
- At least 16 calendar days have passed from the date of the last interim payment determination.
Note: It is recommended that Plan Sponsors stop interim payments at least 60 days prior to an application's Reconciliation Deadline to focus on Reconciliation activities.
- Final rebate information can be received by the Plan Sponsor.
- All user roles, privileges, and user information such as email address must be reviewed and updated as necessary.
- The Reconciliation Deadline has not passed.
Completing Reconciliation Steps: Constraints and Implications
Reconciliation steps must be completed in order - each step must be marked "Complete" to proceed to the next step.
For more information about the constraints and implications of completing the Reconciliation steps and making changes to completed Reconciliation steps, refer to Conditions and Results for Completing Reconciliation Steps.
View the Reconciliation Deadline
For easy reference, the Reconciliation Deadline displays in several locations throughout the RDS Secure Website.
On the Dashboard page, for each of the Plan Sponsor’s applications, the Reconciliation Deadline displays as a column in the Applications table. This is true for In Progress, Completed, and Archived applications, and applications displayed in the Needs Attention view.
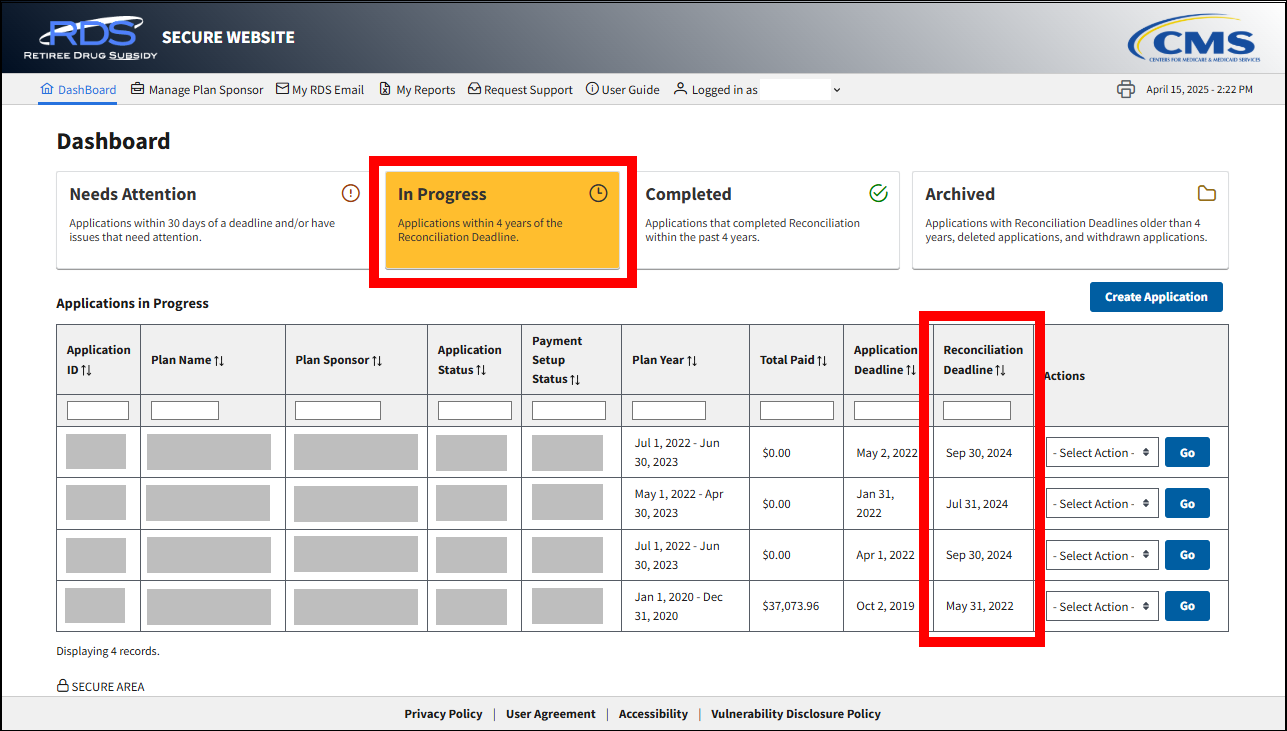
Applications that are within 30 days of the Reconciliation Deadline are displayed in the Needs Attention view of the Dashboard by default.

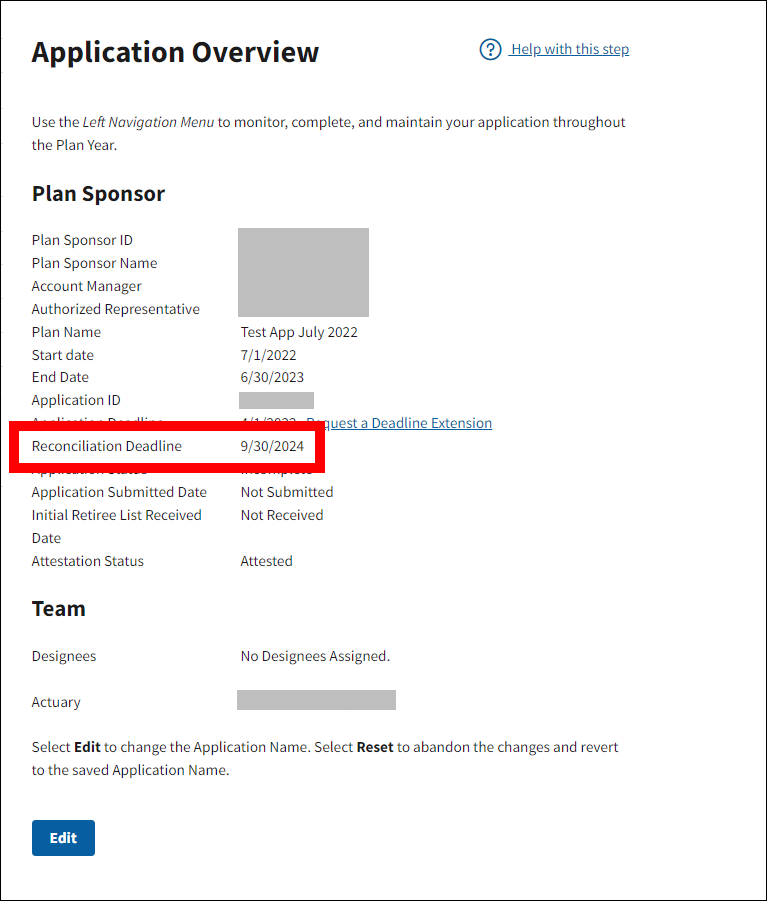
On the Application Overview page, the Reconciliation Deadline displays as a line item in the Plan Sponsor section.
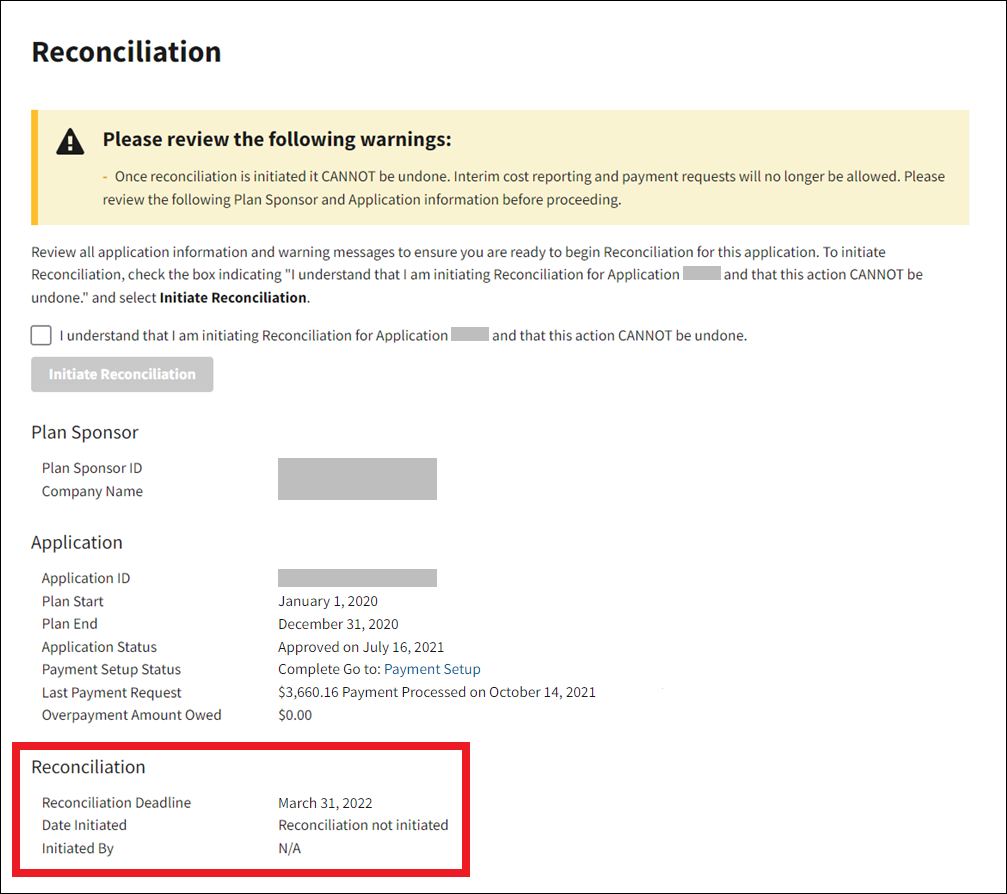
The Reconciliation Deadline also displays as a line item on the Reconciliation page.
Missing the Reconciliation Deadline
For Plan Sponsors that fail to meet their Reconciliation Deadline for a given application and have received interim payments for that application, the sum of those payments becomes an overpayment, and CMS initiates immediate overpayment recovery action.
Plan Sponsors that fail to meet the Reconciliation Deadline for a given application and have not received interim payments for that application will not be eligible for any subsidy payments for that application. CMS' decision whether or not to afford additional time for Reconciliation or to deny a request for extension of the Reconciliation time limit is not subject to appeal.
IMPORTANT: When a user account becomes locked after multiple failed login attempts for any reason—invalid Login ID, Password, or MFA code, or any combination of these—
- CMS’ RDS Center is prohibited by Federal Security Regulations to identify which login requirements were entered incorrectly.
- The user is now required to change their password.
- Passwords can be changed five (5) times in a 24-hour period.
- If a user changes their password the maximum five (5) times and then locks their account again on the same day, the user cannot change their password to unlock their account until 24 hours have passed.
Due to security reasons, the RDS Center does not have the authority to unlock accounts for Secure Website users. As a result, the 24 hours IMMEDIATELY PRECEDING a deadline can be very difficult to obtain remediation regarding account login issues, potentially resulting in a missed deadline and possible loss of subsidy.
User Roles
Reconciliation is completed by a combination of individuals that include a Plan Sponsor's internal resources (such as the Account Manager, Authorized Representative, and Designee with the Request Payment, Report Costs, or View/Send/Receive Retiree Data privilege) along with external resources such as Vendors who may be responsible for cost reporting, as well as the Centers for Medicare & Medicaid Services’ (CMS'), and a Plan Sponsor's banking institution.
Before Reconciliation begins, Plan Sponsors should review the active user roles assigned to each application because each user role has access to various steps within the Reconciliation process. Each user must have a valid email address and should verify their user information before starting Reconciliation.
A Plan Sponsor must have an active Account Manager and an active Authorized Representative. The Account Manager and Authorized Representative are required to complete critical steps during Reconciliation. While the individuals acting in these roles can be changed, the new Account Manager or Authorized Representative must complete the Registration process in order for the Plan Sponsor to complete Reconciliation. The Account Manager and Authorized Representative must maintain active RDS Secure Website user accounts in order for a Plan Sponsor to receive payment.
Federal Security Regulations require that a user log in to CMS' RDS Secure Website (SWS) at least every 180 days to maintain an active account. Users with disabled accounts should refer to Enable Your User Account for more information about maintaining an active account, as well as step-by-step instructions to enable their user account.
Updated Federal security policies also require that each RDS Secure Website account must activate and maintain Multi-Factor Authentication (MFA) prior to accessing the RDS Secure Website. For an overview and step-by-step instructions for managing your Multi-Factor Authentication (MFA) settings, including your text-enabled device number, refer to Multi-Factor Authentication.
A Plan Sponsor may also assign other user roles to perform various functions in Reconciliation, such as Designees with the Request Payment privilege, View/Send/Receive Retiree Data privilege, and Report Costs privilege. For specific instructions on reassigning user roles, refer to User Management.
| Reconciliation Step | Authorized Representative | Account Manager | Designee with Request Payment Privilege |
|---|---|---|---|
| Initiate Reconciliation | Yes | Yes | View only |
| Finalize Covered Retirees - Request CRL | Yes | Yes | Yes Note: Both Request Payment and View/Send/Receive Retiree Data privileges required to access CRL download |
| Finalize Covered Retirees – Approve Covered Retirees | Yes | Yes | View only |
| Finalize Covered Retirees – Reset Reconciliation | Yes | Yes | View only |
| Manage Final Costs | View only | Yes | Yes |
| Review Final Costs | View only | Yes | Yes |
| Review Final Payment Amount | View only | Yes | Yes |
| Banking Information - Review, Update | Yes | Yes | Yes Designee with both Request Payment privilege and Complete Banking Information privilege may complete step |
| Banking Information - Approve | Yes | View only | View only for Designee with both Request Payment privilege and Complete Banking Information privilege |
| Review and Submit | Yes | View only | View only |
Reconciliation Process Overview
Reconciliation is a flow of interconnected steps that guide Plan Sponsors to a successful final payment request. The steps are:
- Reconciliation: Initiate Reconciliation – During this step, the Plan Sponsor indicates to CMS' RDS Center that a Plan Sponsor is ready to submit their application for payment settlement, and that the Plan Sponsor is ready to finalize the Qualifying Covered Retiree List, and will complete all financial accounting for beneficiary costs and Actual Cost Adjustments for this application based on the Covered Retiree List. This step can only be completed after an application's plan year has ended. Once this step is complete, it cannot be undone.
- Reconciliation: Finalize Covered Retirees - During this phase, the Plan Sponsor requests a list of Covered Retirees that includes a record for each Qualifying Covered Retiree for each Benefit Option for each Subsidy Period that has been approved by CMS' RDS Center. Validation of this list is critical because costs can only be reported for the Qualifying Covered Retirees, Benefit Options, and Subsidy Periods listed in the Covered Retiree List. To complete this step, the Plan Sponsor agrees to the Covered Retiree List provided by CMS’ RDS Center.
- Reconciliation: Manage Final Costs - During this step, the Account Manager or Designee with the Request Payment privilege monitors the submission of final cost reports and all reporting sources for the application. Cost Reporters are able to enter final cost reports for the assigned Benefit Options and specify that final cost reporting is complete for this application. This then disallows any further final cost reports from being submitted.
- Reconciliation: Review Final Costs - During this step, the Account Manager or Designee with the Request Payment privilege reviews and confirms all final cost reports for the application, and then indicates their acceptance of all costs at the Benefit Option level, or their rejection of individual cost reports.
- Reconciliation: Review Final Payment Amount - During this step, the Account Manager or Designee with the Request Payment privilege agrees to the final payment request amount before the Authorized Representative approves it.
- Reconciliation: Banking Information – During this step, the Account Manager, the Authorized Representative or Designee with both the Complete Banking Information and the Request Payment privileges obtain final confirmation of the Banking Information associated with the application. Before the final Reconciliation payment can be requested, Plan Sponsors must review the current Banking Information listed in the application and compare it to their records. The Authorized Representative is required to approve or reject the information during this step. This ensures that the Authorized Representative is aware of where the EFT payment is being sent and provides confirmation of that information.
- Reconciliation: Review and Submit – During this step, the Authorized Representative reviews and submits or rejects the Reconciliation final payment request as appropriate. This step may not be initiated until all other Reconciliation steps are marked complete before the application's Reconciliation Deadline.
Step Statuses and Application Statuses during Reconciliation
Each step in the Reconciliation process has a status based on the actions taken in that step. The following table displays the possible Reconciliation step statuses and the corresponding Application Statuses. Application Status is available in the Details box on the Application Overview page and the Reconciliation page.
| Reconciliation Step | Step Status | Application Status Upon Completion of Step |
|---|---|---|
| Initiate Reconciliation | Incomplete, Complete | Reconciliation Initiated |
| Finalize Covered Retirees | Incomplete, Complete | Reconciliation Cost Reporting Opened |
| Manage Final Costs | Incomplete, Complete | Reconciliation Cost Reporting Closed |
| Review Final Costs | Incomplete, Complete | Reconciliation Cost Reporting Closed |
| Review Final Payment Amount | Incomplete, Complete | Reconciliation Cost Reporting Closed |
| Banking Information | Incomplete, Complete, Error - Needs Attention, Rejected | Reconciliation Cost Reporting Closed |
| Review and Submit | Incomplete, Complete, Rejected | Reconciliation Request Completed |
CMS' RDS Center Processing of Reconciliation Payment Requests
CMS' RDS Center processes Reconciliation payment requests after the payment determination is made.
If monies are owed to the Plan Sponsor (the amount is greater than $0), CMS’ RDS Center remits those monies in the form of an Electronic Funds Transfer, just like an interim payment. If the Plan Sponsor has an overpayment (the amount is less than $0) and must remit to CMS’ RDS Center, they will be contacted by email with instructions.
All Reconciliation payment requests are processed as timely as possible.
Maintaining Records
Once the Authorized Representative completes Reconciliation: Review and Submit in the RDS Secure Website, a success message displays on the Reconciliation: Review and Submit page confirming that Reconciliation has been completed. CMS' RDS Center strongly recommends printing this page for your records.
Plan Sponsors should maintain and furnish to CMS or the Office of Inspector General (OIG) upon request the records enumerated in Federal regulations at 42 C.F.R. 423.888(d). The records are maintained for 6 years, or any other period as specified by CMS or OIG, after the expiration of the plan year in which the costs were incurred for the purposes of audits and other oversight activities conducted by CMS to assure the accuracy of the Actuarial Attestation and the accuracy of payments.


